Stroke, spinal cord injury, and traumatic brain injury are common diagnoses treated by neurologic physical therapists (PTs). The course of treatment varies widely based on the severity of the injury and the potential for recovery. For example, a mild stroke, called a Transient Ischemic Attack, may require no therapies. On the other hand, a severe Traumatic Brain Injury or incomplete spinal cord injury may benefit from PT treatment for years if functional gains continue.
By and large, PT approaches to brain injury have one significant commonality: using sensation and feedback to elicit a response. The goal is to provide the brain with a stimulus (input) and train the brain to respond with a consciously controlled meaningful output or appropriate motion. This process has come to be referred to as part of neuroplasticity. Neuroplasticity is the “capacity of neurons and neural networks in the brain to change their connections and behavior in response to new information, sensory stimulation, development, damage, or dysfunction.”

Quite often, the causes of a particular TBI also cause damage to the musculoskeletal system. Most of these orthopedic injuries, whether fractured bones or damaged joints, will heal in a much shorter time than the recovery of the brain itself. Therefore, the healed body may be waiting for months and years to receive instructions from the brain. As the neuroplastic recovery occurs in the central nervous system, time may elapse. The musculoskeletal system will rapidly deteriorate if the Written by Jared Stehr MSPT brain cannot instruct the body to move and interact with the physical forces and stresses of the world that ordinarily keep it well-conditioned. While waiting for the brain to recover, it is imperative to keep the body “ready to go.” This is reminiscent of the classic axiom, “Use it or lose it.” Preventing joint contractures, minimizing the loss of muscle mass, and weighting the skeletal system to stimulate bone density are essential components of treatment.

Specific neurologic therapy will begin in tandem with orthopedic interventions, increasing in duration and intensity as the patient is able to tolerate new challenges. All physical therapy aims to maximize the patient’s purposefully controlled motion. For example, a relearned movement could be turning the head left to right, pointing a finger, taking one step, balancing on one foot, performing a jumping jack, or throwing a ball. As simple motions are mastered, more complex motions are layered with others to complete tasks eventually. These purposefully controlled motions are combined again and again, creating complex movements that are performed to function and interact with the world.
Immediately following a neurologic injury, PT treatment time is primarily spent on balance, gait, and transfer training. These are paramount in a patient’s ability to return home and regain the initial levels of independence. As recovery progresses, the focus changes to more advanced activities of daily living, function, and potentially return to occupation.
A new trend in neuro-PT treatment is high-intensity training, specifically High-Intensity Gait Training (HIGT). By having a patient ambulate vigorously and continuously, many bodily systems are stimulated simultaneously, creating a cascade of physiologic responses that appear more efficient at eliciting recovery than most traditional PT treatments. While conventional neuro-PT treatments focus substantially on the quality of motion, HIGT deemphasizes the quality of motion if it is safe. Research supporting this approach has caused professional PT organizations to revise their Clinical Practice Guidelines, prioritizing using HIGT as a primary treatment for many neurologically involved populations (www.neuropt.org).
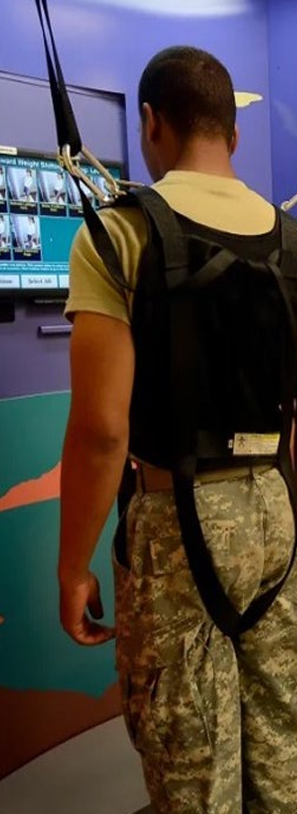
In the proper environment, with the appropriate equipment, HIGT is a treatment option even for severely impacted neurologic patients. Adultsized gait trainers can support the full body weight of a patient if required while keeping them safely within a rolling frame. Both legs may be used to ambulate inside this device, and full weight bearing is encouraged. Ceiling-mounted track systems allow patients to don a full trunk harness and safely walk a circuit while tethered to the installed ceiling track. And finally, if the patient is medically cleared for aquatic therapy, walking in a pool arguably allows the greatest customization of HIGT treatment. The water depth can be chosen to minimize or maximize buoyancy/ impact forces. The viscosity of the water resistively slows motion, lowers fall risk, and provides constant background strengthening. The water’s temperature and enveloping sensation often normalize muscle tone and decrease spasticity. At the moment, the prime limitation of aquatic neuro-PT treatment is access. The availability of suitable therapy pool facilities is low, and the time commitment plus preparation to participate by the patient is high.
Of course, physical therapists do not treat patients in isolation. They are part of a team of allied health professionals, including occupational therapists, speech therapists, recreation therapists, and assistive technologists. Each discipline evaluates patients, determines appropriate goals, and creates a treatment plan. Ideally, each discipline will integrate nonspecialized treatments from the care plans of the other providers as the patient progresses. This reinforces functional gains for the patient. A physical therapist might integrate breathing control into exercises to support what the patient is learning in speech therapy. The occupational therapist might add a simple standing balance task into an activity to reinforce the physical therapist’s goals. A speech therapist could add accurate switch targeting into treatment to follow through with the assistive technologist’s adaptations.
Physical therapy interventions for the neurologically involved patient continue to evolve. In addition to continuously improving traditional techniques, expect to see advancements utilizing robotics, neuro-electric interfacing, and, potentially, exoskeletons. New ideas, continued research, and developing technology are all solid allies for the improved future recovery of individuals with brain injuries.